Submitted by Administrator on Thu, 27/04/2017 - 11:07
Cambridge stem cell scientists have revealed a new mechanism controlling the formation of insulin-producing pancreatic beta cells. These beta cells are the same cells that are damaged and lost in people living with diabetes. With this new understanding, researchers now have the opportunity to improve the production of functional beta cells in the lab which could be used to replace the insulin-producing cells lost in diabetes, offering better treatment options for this disease in future.
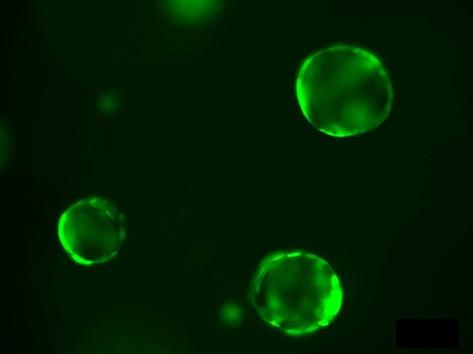
The research team, led by Professor Anna Philpott at the Wellcome Trust–Medical Research Council Cambridge Stem Cell Institute, used developing frogs eggs and mouse pancreas tissue, as well as 3D organoids (lab-grown clusters of cells mimicking the pancreas), to understand how these important cells grow and function during development.
The team found that a critical protein, known as neurogenin3, can be modified by the addition of a phosphate chemical tag. This modification controls the ability of neurogenin3 to regulate the production of new pancreatic hormone-producing cells.
This new finding appears in the journal Developmental Cell, and has the potential to contribute significantly towards improving future outcomes in diabetes. Over 1 in 20 people in the UK are living with diabetes, and 24,000 people with diabetes die early each year. The condition also represents a huge economic burden, with diabetes calculated to cost the NHS £10 billion per year (The Cost of Diabetes Report – Diabetes UK).
“There are a number of methods which we can explore to restore beta cell function in people living with diabetes,” explains Professor Philpott. “The first is to find a way of regenerating the damaged cells directly in the pancreas of diabetic patients. Alternatively, lost cells could be replaced with new beta cells grown from stem cells in the lab.”
“In order to develop new treatments for diabetes, it is essential for us to understand how beta cell formation happens under normal conditions and how we can keep beta cells functioning in diseased states,” said lead author Roberta Azzarelli. “This is what we have achieved in the present study. Our aim now is to use this information to direct new treatment options for people with diabetes.”
Professor Philpott and her team are based in the Department of Oncology at the University of Cambridge, and are part of the pioneering Wellcome Trust-MRC Cambridge Stem Cell Institute at the Cambridge Biomedical Campus. This environment has facilitated this highly collaborative study and provides the ideal platform for Professor Philpott and her team to continue to work towards their goal of understanding pancreatic cell function, ultimately translating this to deliver tangible patient benefit.
The continued support of the MRC, the Wellcome and the Rosetrees Trust has been invaluable in facilitating this research, and is gratefully acknowledged by Anna and her team.
Publication details
R. Azzarelli, C. Hurley, M. Sznurkowska, S. Rulands, L. Hardwick, I. Gamper, F. Ali, L. McCracken, C. Hindley, F. McDuff, S. Nestorowa, R. Kemp, K. Jones, B. Göttgens, M. Huch, G. Evan, B. Simons, D. Winton and A. Philpott. Multi-site Neurogenin3 phosphorylation controls pancreatic endocrine differentiation. Developmental Cell. DOI: 10.1016/j.devcel.2017.04.004

