Submitted by Administrator on Tue, 29/11/2016 - 12:40
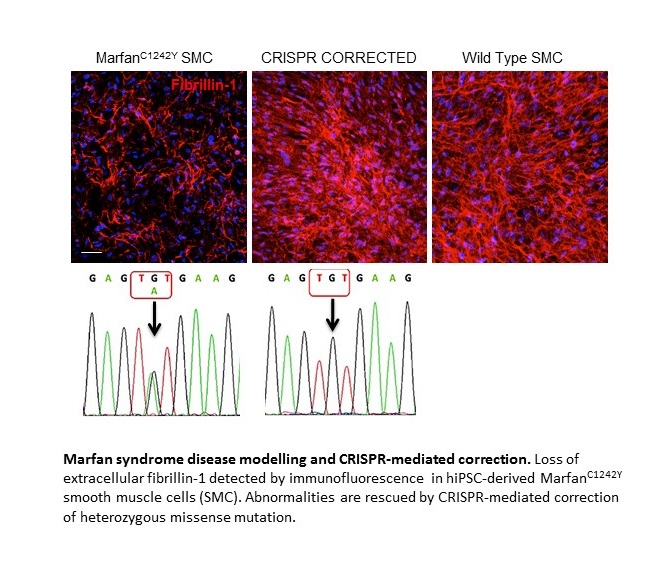
The Sinha Lab, funded by the British Heart Foundation, has created, for the first time, blood vessel tissues in a petri dish which mimic Marfan syndrome in human arteries. The study is published in Nature Genetics.
An estimated 13,000 people in the UK have Marfan syndrome, which is caused by mutations in a gene known as fibrillin-1.
People with Marfan syndrome often go on to have a thoracic aortic aneurysm (TAA), where the main artery leading away from the heart balloons and can cause a life-threatening rupture.
Currently the only treatment that prevents aortic rupture for Marfan patients suffering from a TAA is to have open-heart surgery to replace the damaged section of the aorta.
SCI researchers have now used these blood vessel models to gain more understanding of how the inherited disease can lead to fatal aneurysms. Their results provide insights into why clinical trials of drugs to treat the disease have so far been largely unsuccessful. The team now hope to use the lab-generated vessel cells to test drugs for people with Marfan syndrome.
Dr Sanjay Sinha, a BHF Senior Research Fellow, who led the research said: "We now hope to use our newfound understanding of the way that these aneurysms develop to find new drugs to prevent these fatal aneurysms from occurring."
Read more: BHF
Publication details:
Granata A, Serrano F, Bernard WG, McNamara M, Low L, Sastry P, Sinha S. An iPSC-derived vascular model of Marfan syndrome identifies key mediators of smooth muscle cell death. Nature Genetics (2016) doi:10.1038/ng.3723

