Haematopoietic stem cells and malignancies
Laboratory: Cambridge Stem Cell Institute, Jeffrey Cheah Biomedical Centre
Departmental Affiliation: Haematology
Biography
Ingo Ringshausen studied medicine at the Johannes Gutenberg University in Mainz/ Germany and London/ Canada. After his graduation in 1999 he started his medical training in Internal Medicine and Haematology/ Oncology at the Technical University in Munich. Between 2003 and 2006 he joined the group of Gerard Evan at UCSF on a research fellowship. After his board certification in 2010 he became a Consultant in the Department of Haematology/ Oncology in Munich and subsequently an independent group leader.
In 2014 he joined the Department of Haematology in Cambridge and is now appointed as Consultant Haematologist at Addenbrooke’s hospital and a Principal Investigator at the CSCI.
Funding
Cancer Research UK, Kay Kendall Leukaemia Fund
Research
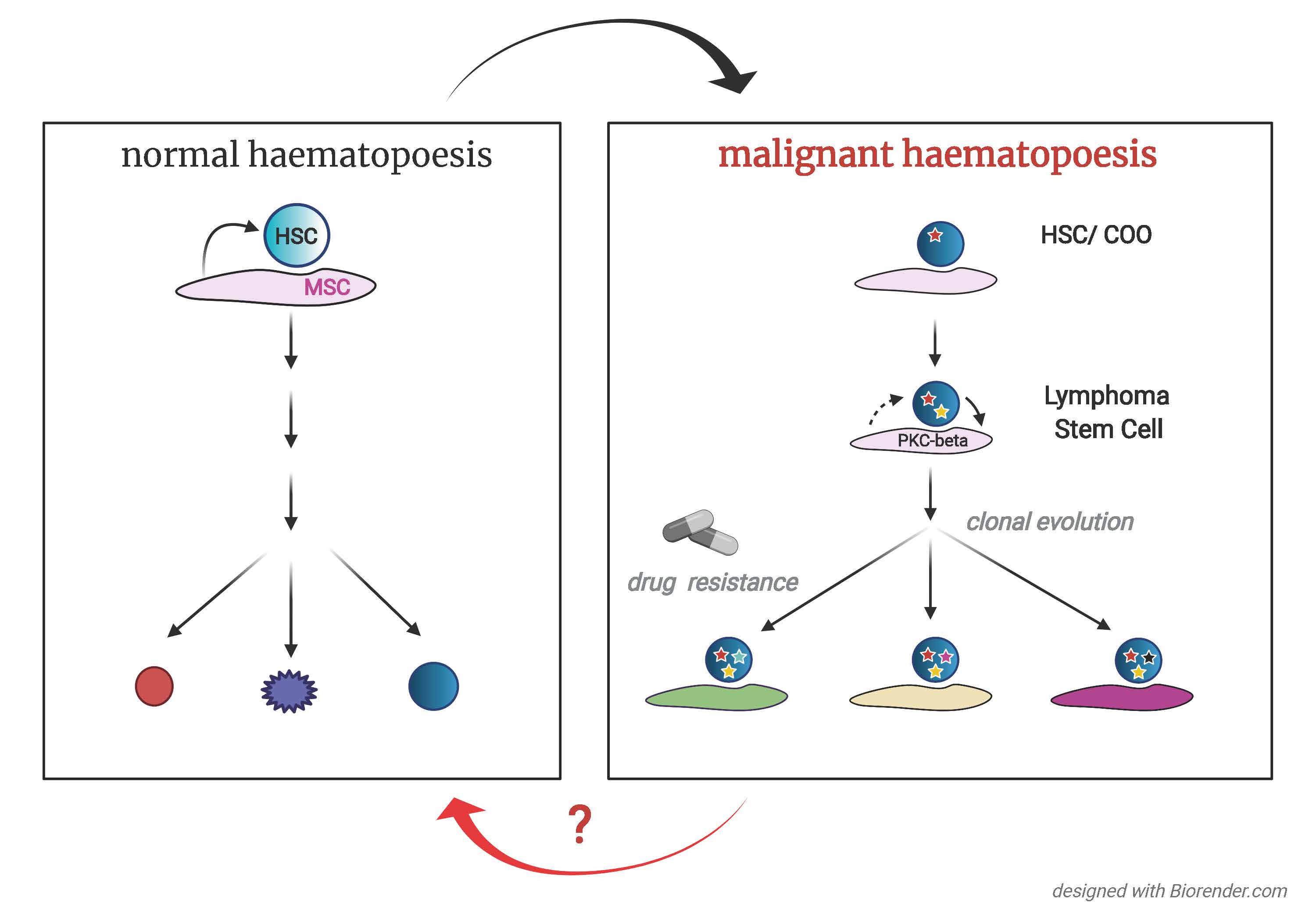
Our research group studies the molecular processes underlying the cross-communication between normal and malignant haematopoiesis and their microenvironment. It has recently been shown that CD34+ CD38- HSPCs can contribute to oncogenic transformation into mature B cell malignancies, such as Chronic Lymphocytic Leukaemia. Similar to normal cells, tumour cells require signals from their surrounding environment to survive and proliferate. Our work has identified vulnerabilities of cancer cells in this cross-talk, which can be exploited therapeutically. We have identified kinases activated in bone marrow stroma cells, which are essential for tumour-associated inflammation and tumour progression. We are now (1) focussed on defining how tumour-host interactions are modulated along tumour-evolution, from the Cell-of-Origin (COO) to lymphoma-stem cells to therapy-refractory disease. These studies are important to (2) fully understand lymphomagenesis and how the tumour microenvironment contributes to drug resistance and minimal-residual disease (MRD) following systemic anti-cancer therapies.
In parallel (3), we study how the tumour-remodelled bone marrow microenvironment affects normal HSC function and contributes to secondary bone marrow failure. Therapeutic interventions with these cross-talks could be exploited to maintain HSC function and thereby eliminate tumour cells, while maintaining and improving immune functions in patients with B cell malignancies.
Ringshausen Group photo
Plain English
Similar to normal blood stem cells, malignant cells from patients with B cell lymphomas require signals from their surrounding environment for cell survival and proliferation. Thus, benign bystander cells provide crucial support for malignant cells, mediated by direct cell-cell contact and soluble factors. Understanding these cell-cell communications from a molecular viewpoint opens new directions to treat blood-born malignancies. Specifically, we want to understand: 1. How this cell-cell communication changes over time? Are malignant cells from patients with relapsed disease equally dependent on these signals? 2. How does this communication between malignant cells and their micro-environment affects the function of normal haematopoietic stem cells and the production of normal blood cells?