Submitted by Laura Puhl on Thu, 24/08/2023 - 16:00
Scientists have created a new test for identifying people at risk of developing acute myeloid leukaemia and related cancers, years before they do. The new platform, ‘MN-predict’, will allow doctors and scientists to identify those at risk and to design new treatments to prevent them from developing these potentially lethal cancers.
Researchers at the Wellcome-MRC Cambridge Stem Cell Institute (CSCI), the University of Cambridge’s Department of Haematology, and Instituto de Investigación Sanitaria del Principado de Asturias (ISPA) analysed data from more than 400,000 individuals participating in the United Kingdom Biobank.
Using this data, the scientists have created "MN- predict," a platform for predicting the risk of developing blood cancers such as acute myeloid leukaemia, myelodysplastic syndromes and myeloproliferative neoplasms over a 10-15-year period. This test, now available in NHS clinics, requires patients to provide a blood sample from which DNA is extracted for limited sequencing, alongside basic blood cell counts. With this information, MN-predict identifies those at high risk of any of these cancers and can be used in specialist clinics for leukaemia prevention.
Professor George Vassiliou, senior author of the study, said, “We all know that prevention is better than cure, but it is not easy to prevent diseases like leukaemia without knowing who is at risk. MN-predict makes it possible to identify at-risk individuals, and we hope it can become an essential part of future leukaemia prevention programmes.”
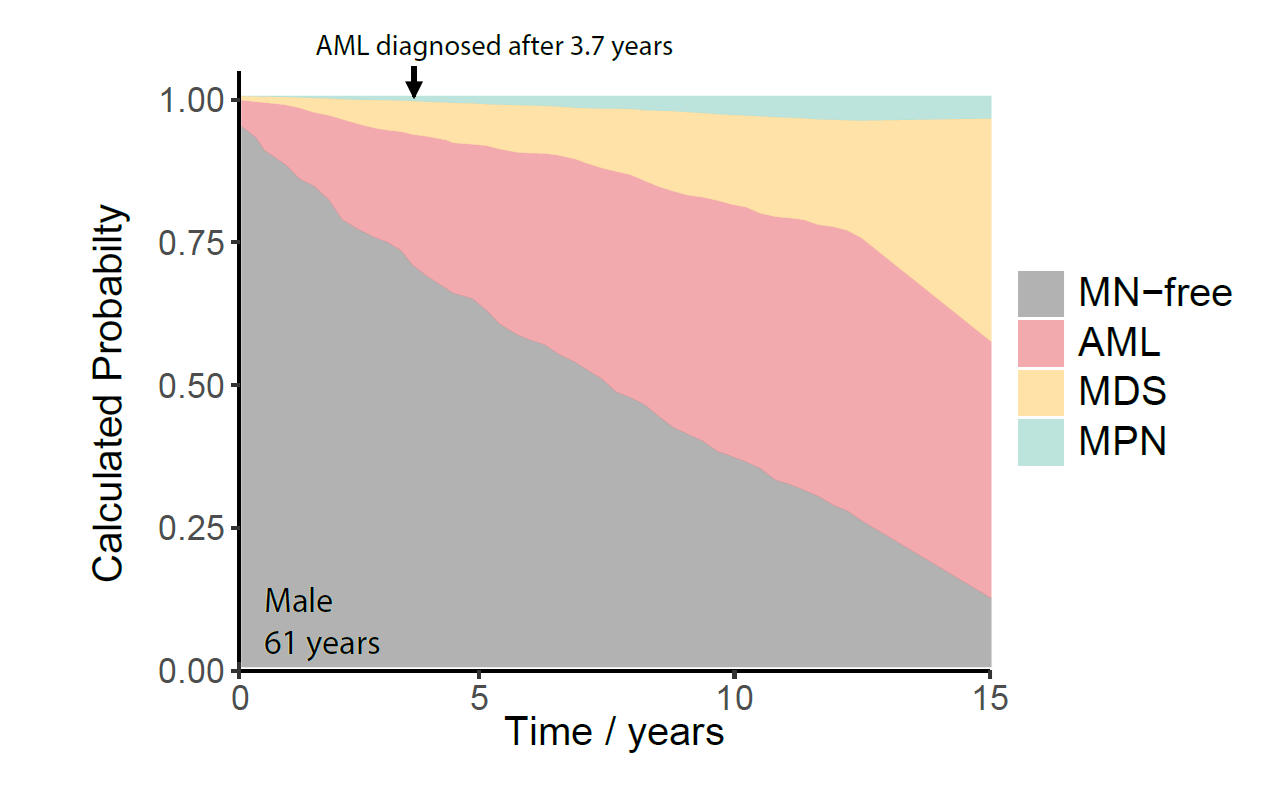
MN-Predict example calculations
MN-Predict calculates the probabilities of developing acute myeloid leukaemia (AML), myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPN) over 15 years based on limited blood DNA sequencing data and simple blood tests. This example depicts these probabilities for a 61-year-old man, who went on to develop AML 3.7 years after blood sampling.
The myeloid neoplasms are a group of related cancers encompassing acute myeloid leukaemia, myelodysplastic syndromes and myeloproliferative neoplasms. Treatments for these cancers have improved in the last few years, but most cases remain incurable.
In the last few years, scientists discovered that these cancers develop over decades through the accumulation of DNA mutations in blood stem cells, the cells responsible for normal blood formation. These mutations encourage these stem cells to grow faster than normal and, as more mutations accumulate, they can progress towards leukaemia. Thankfully, whilst mutations that promote cell growth are common, leukaemia develops only in a small minority of cases. Identifying these cases early on helps efforts to prevent the cancers from developing.
"We hope that MN-predict will help clinicians to identify people at risk of myeloid cancers and use novel treatment to prevent the cancers from developing.”
- Dr Muxin Gu, first author