Submitted by Administrator on Wed, 18/04/2018 - 12:39
Two research projects are underway at the University of Cambridge that are seeking to find new ways to treat acute myeloid leukaemia (AML), a highly aggressive blood cancer that currently only one in five people survive for longer than five years after diagnosis.
Around 35 people are diagnosed with AML in Cambridgeshire each year. It can affect anyone of any age, but the majority of patients are over 60. Saturday 21 April is World AML Awareness Day.
The two projects, which will run over three years, have received £535,000 in funding from the blood cancer research charity Bloodwise.
Researchers led by Professor Brian Huntly and Dr George Vassiliou at the Wellcome-Medical Research Council Stem Cell Institute are tracking the genetic changes that blood cells go through early in their development into leukaemia cells to see whether treatments could be created to prevent AML from fully progressing.
Professor Tony Kouzarides’ team at the Wellcome/Cancer Research UK Gurdon Institute are designing a drug to target an enzyme that leukaemia cells depend on to grow.
Dr Alasdair Rankin, Director of Research at Bloodwise, said: “Survival rates for AML remain tragically low, with current treatments only curing a small proportion of patients. Intensive chemotherapy, often combined with a stem cell transplant, offers the best chance of a permanent cure, but many patients are too elderly to undergo this gruelling treatment, which can have fatal side effects even before it has the chance to work. These exciting research projects at the University of Cambridge are looking to find gentler and more effective treatments. ”
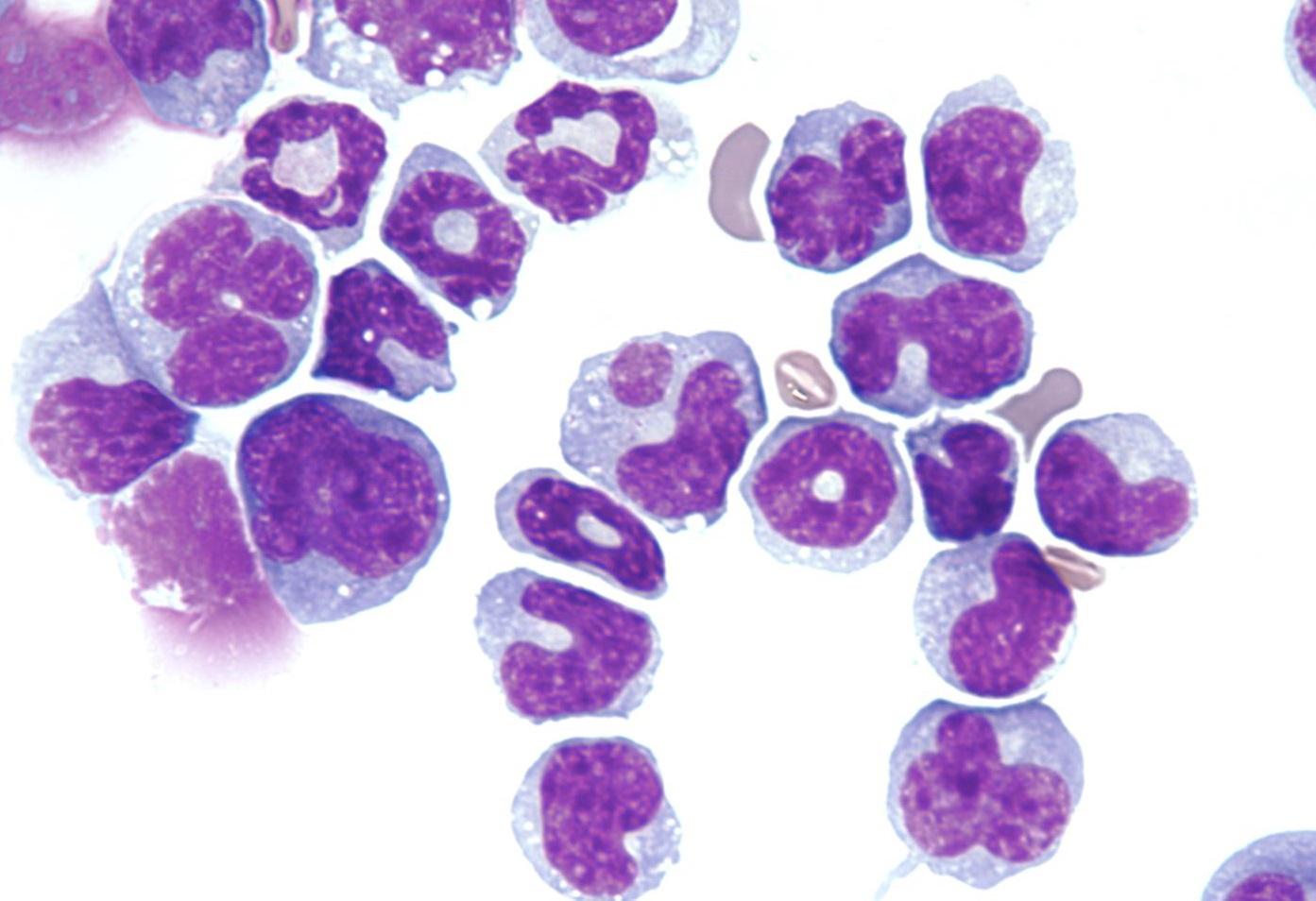
AML affects a family of blood cells called myeloid cells, which include certain types of white blood cells, red blood cells and platelets. The team at the Cambridge Stem Cell Institute are studying mice with AML to see how early genetic mutations in healthy myeloid cells can kick-start the accumulation of additional DNA damage, leading to the growth of full-blown leukaemia cells with multiple genetic mutations.
Professor Brian Huntly said: “Effective new treatments for AML are desperately needed. By studying which genetic mutations are critical to the development of AML in its early stages, we will identify potential drug targets that could allow earlier and more successful treatment intervention in this highly aggressive disease.”
Professor Tony Kouzarides’ team has shown that genetic material, called RNA, plays a critical role in AML cells’ growth. RNA molecules act as ‘messages’ from the genetic instructions contained in the cell’s DNA, which are then translated into the proteins that carry out cell functions.
Not all RNA molecules become proteins - many remain as RNA molecules and play a role in regulating cell behaviour. RNA molecules are often modified by enzymes in the cell and sometimes this means that the genetic ‘message’ is hijacked, which can lead to cancer. The Gurdon Institute team have discovered that AML cells rely on an RNA modifying enzyme called DIMT1 to grow.
Professor Tony Kouzarides said: “We’re trying to understand why this specific enzyme is so influential in the growth of AML. If we can design a molecule that can block its activity, we may be able to create a new targeted drug for AML.”

