Submitted by Laura Puhl on Thu, 09/06/2022 - 20:21
Our body produces one trillion new blood cells each day, a process driven by rare haematopoietic stem and progenitor cells (HSPC) inside the bone marrow. A new paper demonstrates that even rarer HSPCs with unique features also exist in other human organs. This work, from the Wellcome-MRC Cambridge Stem Cell Institute (CSCI) and the Department of Haematology at University of Cambridge and published in the journal Blood on 9 June opens the door to new ways to detect and treat disease in the future.
Tapping the source
In healthy adults, over 99% of mature blood cell production occurs inside the marrow of our bones. Very few of the stem cells that produce all blood cells can also be found outside the bone marrow, where they lurk in tissues like the spleen, or within the blood that circulates throughout the body. While scientists have long known this, the composition and function of these cells have largely remained a mystery.
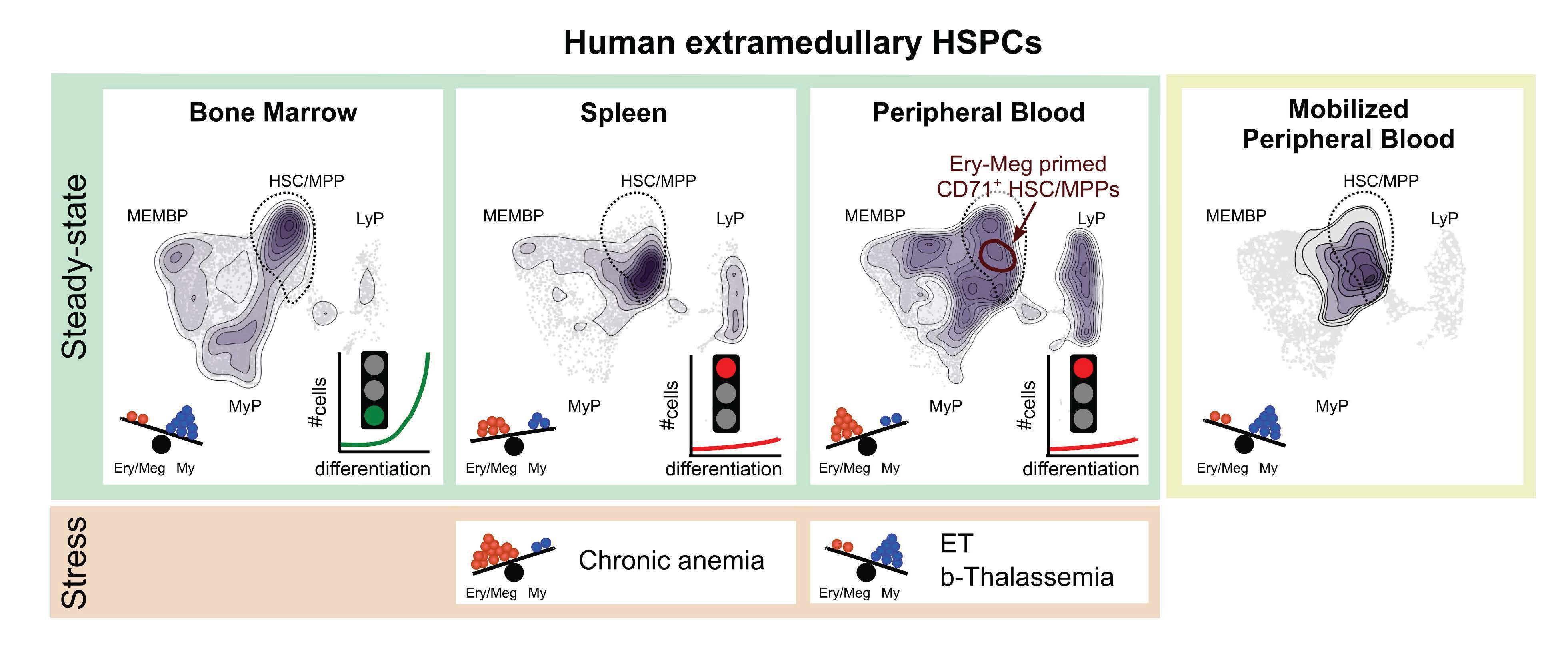
Due to the rarity of HSPCs in tissues outside the bone marrow, it has previously been a challenge to source a large enough amount to study them effectively. Now, however, with the explosion of technologies which can probe individual cells, the possibilities have expanded, allowing a more detailed look into rare stem cells and their potential applications. Joint first authors of the study, Dr Nicole Mende and Dr Hugo Bastos of the Laurenti Lab at CSCI, used cutting edge single cell technologies to compare the properties of HSPCs across three different tissues: blood, spleen, and bone marrow. The team made two major findings.
A hidden reservoir
First, whereas HSPCs in the bone marrow act as the powerhouse of blood production, the ones found outside the bone marrow do not participate in making blood in healthy people. However, when the researchers studied patients suffering from chronic anaemia, they found that HSPCs inside the patients’ spleens were actively producing new red blood cells. These pockets of HSPCs found outside the bone are therefore reservoirs capable of rapidly making mature blood cells only when the need for blood cells is substantially increased, such as in disease.
Dr Nicole Mende, lead post-doctoral researcher says, “There is so much that we do not know about what happens in our bodies, simply because sampling human tissues is invasive. In this work, we were lucky to use spleen samples that were otherwise unutilised by-products of clinical organ transplantation or life-saving surgeries. We are thankful to those who have consented for us to use these tissues, making these new discoveries possible. This work lays the foundation for better understanding our body’s response to chronic anaemias and for finding new treatments to alleviate these debilitating diseases.”
Signalling errors in blood production: diagnostic and research potential
The second finding from the team was that HSPCs normally circulating in the blood are broadly different to those found in the bone marrow. Specifically, circulating HSPCs are specialised to make red blood cells, while bone marrow HSPCs favour production of specific immune cells called myeloid cells. Interestingly, increased presence of HSPCs within the blood circulation now instructed to produce myeloid cells was found to be indicative of something going wrong with blood production, such as in anaemia or other blood disorders.
During the course of this research, the team was able to compile a sizeable amount of data, filling a gap in the research community. Now, future research can use this as a database to inform future basic and applied studies. Dr Hugo Bastos, lead bioinformatician on the study, noted, “Not only have we analysed what occurs across the body physiologically, but we also provide a high-resolution description of the most used stem cell source in clinical transplantation, pharmacologically mobilised blood. Understanding its composition is a cornerstone to improve outcomes of blood stem cell transplantation.”
On using these research findings in the future, Dr Laurenti, Assistant Professor, Sir Henry Dale Fellow at CSCI, and senior researcher on this study, is hopeful that the new tools available will help solve more haematological mysteries, and be used to improve detection of disease. She comments, “Blood is routinely sampled during clinical management, but the diagnostic potential of blood HSPCs has remained largely untapped. This is simply because we were lacking the tools to go down to the level of resolution we needed to track down these cells, and the samples to do so. It’s been really fascinating to begin to unravel how human blood stem cells behave outside of their normal home. Do they contribute to resolving inflammation in the different organs? Do they somehow facilitate disease? We still do not know. But our work already provides an important base for novel clinical applications. In the future, if researchers can detect certain changes in HSPCs with just a blood sample from the patients, this could signal to doctors that something is amiss and could lead to earlier treatment.”

